Polycystic Ovary Syndrome (PCOS) is a common hormonal condition affecting people of reproductive age. It influences hormone levels, menstrual cycles, metabolism, and fertility. While PCOS is a lifelong condition, medical care combined with lifestyle guidance can significantly reduce symptoms and improve long-term health outcomes.
Understanding how PCOS is diagnosed and treated empowers individuals to take informed, proactive steps toward better health.
What Is Polycystic Ovary Syndrome (PCOS)?
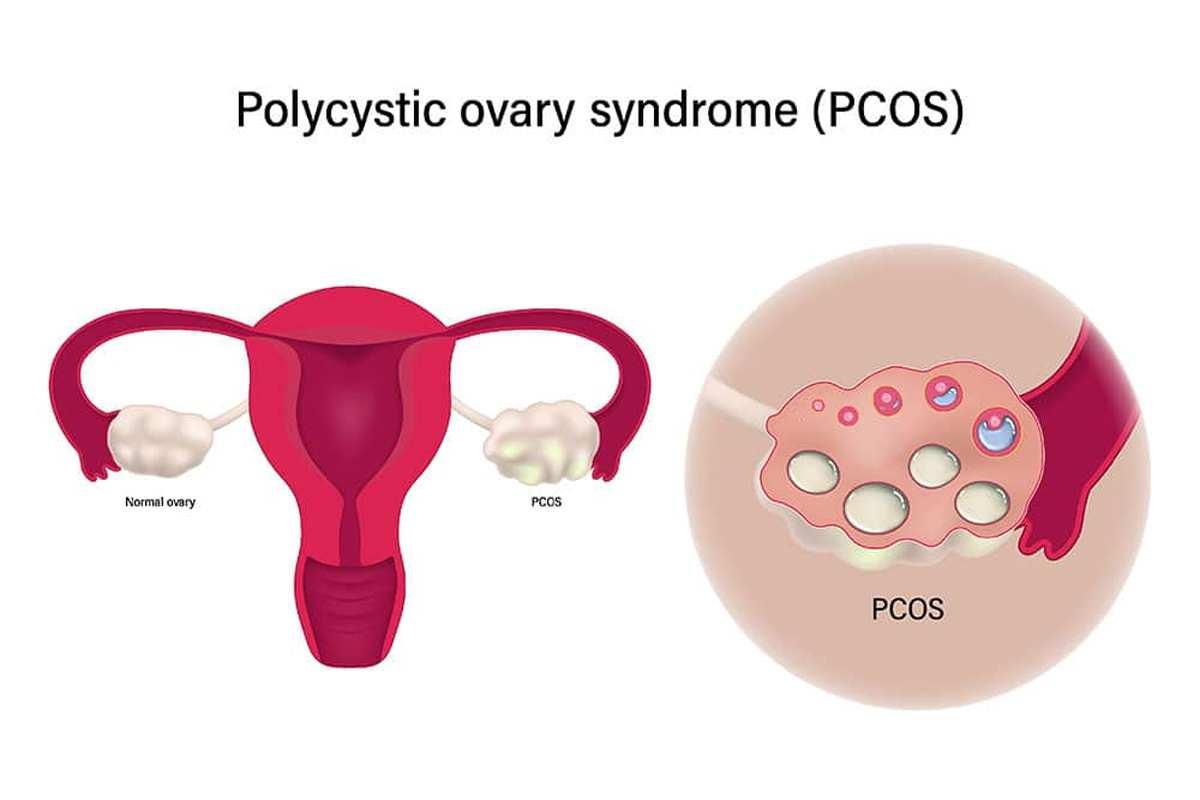
PCOS is a hormonal disorder characterized by irregular ovulation, excess androgen levels, and ovarian changes. Not everyone with PCOS experiences cysts on the ovaries, which is why diagnosis relies on a combination of symptoms and clinical findings.
Common Features of PCOS
-
Irregular or absent menstrual periods
-
Elevated male hormones (androgens)
-
Multiple small follicles on the ovaries
-
Insulin resistance
Common Symptoms of PCOS
Symptoms vary widely and may change over time. Some individuals experience mild effects, while others face more disruptive symptoms.
Physical and Hormonal Symptoms
-
Irregular or missed periods
-
Excess facial or body hair growth
-
Acne or oily skin
-
Thinning scalp hair
-
Weight gain or difficulty losing weight
Metabolic and Emotional Effects
-
Insulin resistance or prediabetes
-
Fatigue
-
Mood changes, anxiety, or depression
How PCOS Is Diagnosed
There is no single test for PCOS. Diagnosis is usually based on clinical criteria, medical history, and laboratory findings.
Diagnostic Tools Include
-
Blood tests to assess hormone levels
-
Pelvic ultrasound to examine ovarian structure
-
Menstrual history evaluation
-
Metabolic screening for glucose and cholesterol levels
Medical Treatment Options for PCOS
Medical care focuses on managing symptoms rather than curing the condition. Treatment is tailored based on individual goals, such as menstrual regulation, symptom control, or fertility support.
Hormonal Treatments
-
Combined oral contraceptives to regulate periods and reduce androgen levels
-
Progesterone therapy to protect the uterine lining
-
Anti-androgen medications to reduce hair growth and acne
Metabolic Support
-
Insulin-sensitizing medications to improve glucose regulation
-
Monitoring and management of cholesterol and blood pressure
Fertility-Focused Treatments
-
Ovulation-inducing medications
-
Hormonal therapies guided by reproductive specialists
The Role of Lifestyle Changes Alongside Medical Care
While medications play a central role, lifestyle interventions enhance treatment effectiveness.
Supportive Lifestyle Strategies
-
Balanced nutrition emphasizing whole foods
-
Regular physical activity
-
Stress management and sleep optimization
-
Gradual, sustainable weight management if advised
Medical professionals often integrate lifestyle guidance with prescriptions for more consistent symptom control.
Long-Term Health Monitoring
PCOS is associated with several long-term health risks, making ongoing medical follow-up essential.
Conditions That Require Monitoring
-
Type 2 diabetes
-
Cardiovascular disease
-
Endometrial hyperplasia
-
Mental health concerns
Early detection and routine checkups help reduce complications and support overall well-being.
When to Seek Medical Care
Consult a healthcare provider if you experience:
-
Persistent menstrual irregularities
-
Symptoms of excess androgen (hair growth, acne)
-
Difficulty conceiving
-
Sudden weight changes or fatigue
Early intervention allows for more effective symptom management and prevention of complications.
Frequently Asked Questions (FAQs)
1. Can PCOS be cured permanently?
PCOS cannot be cured, but symptoms can be effectively managed with medical treatment and lifestyle support.
2. Does everyone with PCOS have ovarian cysts?
No. Some individuals meet diagnostic criteria without having visible cysts on ultrasound.
3. Is PCOS only a reproductive condition?
No. PCOS also affects metabolism, cardiovascular health, and mental well-being.
4. Can PCOS symptoms change with age?
Yes. Symptoms may evolve over time, especially with hormonal changes or treatment.
5. Is medication always required to manage PCOS?
Not always. Treatment plans vary based on symptoms, health risks, and personal goals.
6. Can PCOS increase the risk of other diseases?
Yes. PCOS is associated with higher risks of diabetes, heart disease, and endometrial conditions.
7. How often should someone with PCOS see a doctor?
Regular follow-ups are recommended, typically annually or more often if symptoms change.